The 2022 Lockton National Benefits Survey will be launching in Q1 2022 with a report made available to those who participate early summer 2022. Reach out to your Lockton contact for more information or if you would like to participate.
Lockton’s third annual national benefits survey can help employers compare their benefits strategies with those of other employers — providing benchmark data, highlighting trends and illuminating new ideas.
Nearly 1,450 U.S. employers responded to the 2021 survey*, which is the first to capture responses that reflect a full year of operations in the pandemic environment. At a high level, it tells us that employers were slow to make visible changes in their benefits, but they’re using behind-the-scenes strategies to manage costs, and they’re enhancing benefits to address pandemic-driven needs.
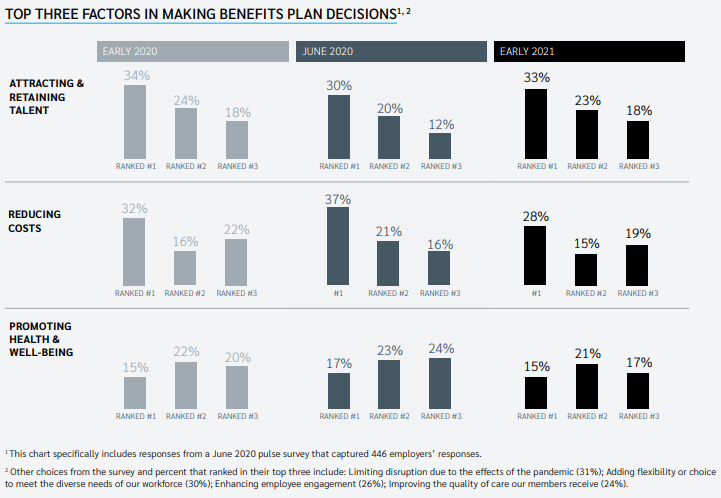
01 | Attracting and retaining employees is the top factor in benefits decision-making, with cost considerations in second place
Attracting and retaining talent is the primary factor in benefits decision-making; 74% of employers ranked it among the top three. This is balanced by cost considerations at 61%, while promoting employee health and well-being rounds out the top three considerations at 53%. In a new question for 2021, almost a third of employers said limiting disruption due to the effects of the pandemic was one of their top three decision-making factors.

02 | More work perks are on the way
This was the first time we measured the following work perks, and we expected them to become more prevalent given the pandemic. If employers follow through on their plans for 2022, 27% will be offering a home office/technology stipend, and 51% will offer a cell phone stipend.
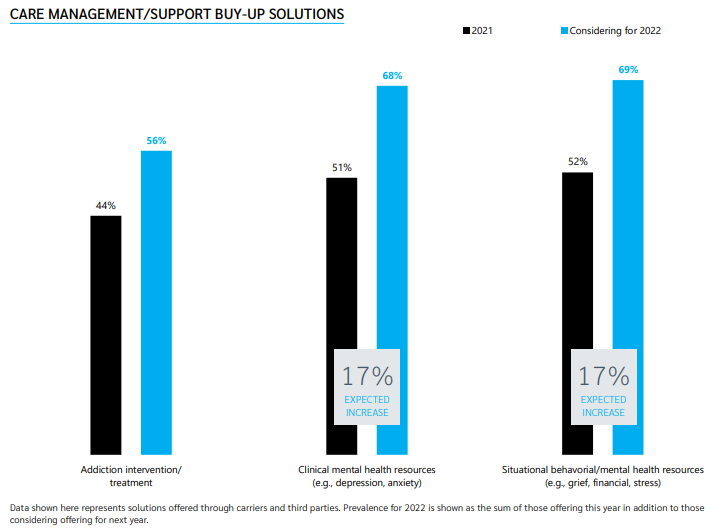
03 | Care and disease management interest continues, especially for mental health
Employers indicated a heightened interest in exploring behavioral health and mental health solutions, investing in buy-up solutions in this space that go above and beyond standard programs.
Almost 70% of employers are offering or considering situational and clinical mental/behavioral health services, and 56% are offering or considering addiction intervention/treatment.
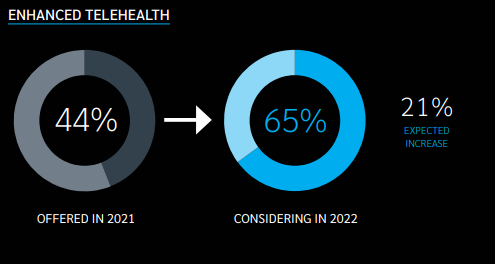
04 | Pandemic forces increased the offering and uptake of telehealth services
Likely driven by the increased offering and uptake, employers are expanding their telehealth solutions. While more than 90% already had some sort of primary care telehealth solution in place, 65% of them are considering enhancing their benefits to expand clinical capabilities beyond acute care, such as chronic condition management, specialist visits and behavioral health.
Lockton’s Infolock® data reveals traditional providers and consumers embraced telehealth solutions during the pandemic, with 67 visits per 1,000 members in April 2020, versus 4 per 1,000 early in 2020. As restrictions ease and traditional providers welcome patients back into their offices, that number is leveling out to about 40 per 1,000 members.
Lockton’s 2021 survey is available to participating organizations and also addresses trends in benefits communications, wellness programs, medical plan design, voluntary benefits, purchasing efficiencies and targeted care management solutions.
Your Lockton team can help you understand how recent survey findings can provide insight for your benefits strategy.
 Download article (opens a new window)
Download article (opens a new window)
*The Lockton Benefits Survey launched Feb. 3, 2021, and closed March 25, 2021.

