While reserving capacity for Covid-19 patients was crucial to cope with the virus outbreak it has prevented diagnostics and treatment for other diseases. Addressing this backlog is a matter of urgency and remote consulting has to be part of the solution.
In the 15 weeks following the lockdown on 23rd March 2020, 2.7 million people were not screened with FIT/FOBT, breast screening mammogram, and cervical smear, as they would otherwise have been, according to HCA Healthcare UK. Urgent suspected cancer referrals were down 301,000. This means that a growing population remains undiagnosed. This is a serious matter since the more progressed the diagnosed cancer is, the lower the chances of a successful treatment.
In the UK, delays to cancer diagnosis and treatment due to coronavirus are expected to cause at least 7,000 additional deaths and up to 35,000 extra cancer deaths, according to healthcare experts (opens a new window). This is despite the fact that the NHS England and the independent sector joined forces to create safe spaces to allow complex cancer treatment and surgery to continue, for both private and NHS patients.
These estimates are driven by concerns that routine screenings, urgent referrals and treatments have been delayed or cancelled during the pandemic outbreak. The study, conducted by DATA-CAN, the Health Care Research Hub (HDR UK) for Cancer, modelled different outcomes depending on how long services take to get back to normal levels.
The NHS backlog
The UK’s National Health System (NHS) is restarting (opens a new window) a wide range of services either paused or stopped when the pandemic struck but the waiting list for routine procedures has grown to more than 4 million during the virus outbreak, and the situation is likely to get worse.
NHS organisations face further capacity constraints with hospitals, for example, having to run at much lower rates of occupancy than normal as procedures need to reflect social distancing rules and staffing constraints.
The NHS Confederation, the membership body for organisations that commission and provide NHS services, suggested (opens a new window) that the NHS waiting list could reach 10 million by the end of 2020. The organisation warned that this number could rise further if there is a second wave of COVID-19 and a lack of treatment or a vaccine.
Cancer in the UK
There are around 367,000 new cancer cases in the UK every year, that's around 1,000 every day (2015-2017), according to Cancer Research UK (opens a new window), a cancer research and awareness charity.
Among the most prevalent cancer forms are breast, prostate, lung and bowel cancers, according to the statistics.
In the UK there are around 165,000 cancer deaths every year and around 450 per day (2015-2017). Cancer accounts for more than a quarter (28%) of all deaths in the UK. In females, there were around 77,700 cancer deaths in 2017 in the UK while in males this number was a bit higher at around 88,900. Every four minutes someone in the UK dies of cancer.
Survival for some of the most common types of cancer is more than three times higher when the disease is diagnosed in the earlier stages, according to figures by Cancer Research UK (opens a new window).
Reducing the backlog
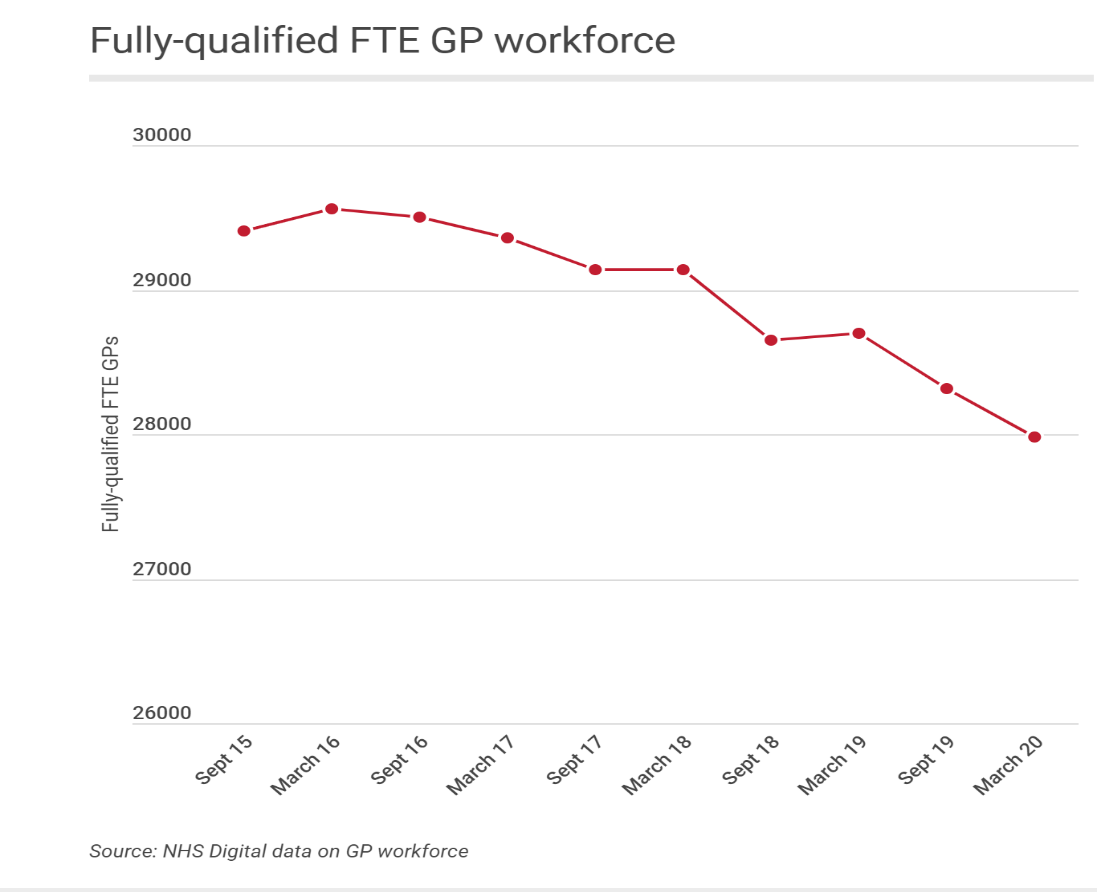
But how are surgeries going to cope with the backlog as they try to get back on their feet after COVID-19? Statistics published by NHS digital (opens a new window) for England on May 28, 2020 showed that the number of fully qualified general practitioners (GPs) shrank 2.5% year on year in March to 27,985 full-time equivalent (-712).
Nevertheless, an impressive rollout of remote telephone and video consulting which occurred as a result of the pandemic will mark a paradigm shift in how healthcare is delivered in the UK.
The NHS has accelerated (opens a new window) its work to provide online consultations during the pandemic so that patients can digitally contact their GP surgery and get health information, advice and help for example through the NHS App.
NHS England and NHS Improvement have asked general practices to move toward a “total triage” model to reduce avoidable footfall during the pandemic.
Patients have come to understand that it is not always necessary to be examined in person and that many health matters can be dealt with remotely.
For the past 3 years, our colleagues at Dr Morton’s (opens a new window), for example,have made consultant gynaecologists available by telephone, email and video through their medical helpline.
Advice to businesses
As part of their duty of care towards employees, businesses should understand that the need to provide expert care is now more pressing than ever. Apart from a delay in diagnostics and treatment for diseases other than Covid-19, the past months have caused additional stress to workers as they had to perform their tasks from home while potentially also caring for children or relatives.
Businesses should therefore offer reassurance to staff that support for both mental and physical issues is available, that they should not delay seeking help due to the pandemic, and emphasise that early diagnostics are key.
For further information, please contact:
Rachel Lewis, Senior Benefit Consultant
Tel: +44 (0)20 7933 1179 | Email: Rachel.Lewis@uk.lockton.com (opens a new window)


